Lyme and Other Tick-Borne Diseases/Conditions Awareness Month Begins May 1
As the snow melts and the trees begin to bloom, it isn’t just springtime – it’s the start of Tick Season in Colorado.
Governor Jared Polis, Chaffee County, the City of Salida, and the town of Buena Vista have all proclaimed the Month of May as Lyme and Other Tick-Borne Disease/Conditions Awareness Month for 2023.
With more people heading out to participate in all the activities that warmer weather brings to our valley, they’ll be outside in greater numbers and so will ticks. Though ticks may be active year-round, “tick season” is upon us and it is time to ELEVATE awareness. Both residents and visitors are exposed to ticks and tick-borne diseases (TBD) through work, play, outdoor recreation, and travel. Pets, horses, and other livestock are also at risk for tick-borne diseases and can put humans at greater risk as well.
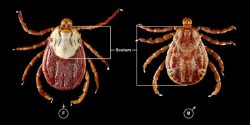
Ticks associated with Rocky Mountain Spotted Fever.Image courtesy of Lyme Disease Association.
The rate of Lyme disease and other tick-borne infections continues to spread rapidly across the United States. The U.S. Environmental Protection Agency (EPA) uses the incidence of Lyme disease as one of the monitors of climate change. The Centers for Disease Control and Prevention (CDC) now estimates case numbers for Lyme disease to be over 476,000 across the United States annually. This number does not include the other 15 reportable tick-borne diseases that people can acquire throughout the country.
Many diseases are not reportable for humans at the state level leaving rates of local infections for many TBDs unknown. The Companion Animal Parasite Council reports a continuing upward trend for Lyme disease, ehrlichiosis, and anaplasmosis cases in Colorado dogs since 2012.
In addition to Lyme disease, ticks can transmit many other germs (bacteria, viruses, and protozoan) that can cause many serious and sometimes fatal diseases. Colorado Tick Fever, Spotted Fever Rickettsiosis (such as Rocky Mountain Spotted Fever), Tularemia, Babesiosis, Ehrlichiosis, Anaplasmosis, Tick-Borne Relapsing Fever, and others can be acquired across the country and around the world. Ticks can also transfer various substances in their saliva that may lead to tick paralysis, alpha-gal syndrome, and others. Ticks can transmit several germs that can result in multiple diseases from a single bite.
Colorado is home to nearly 30 species of ticks. Other species of ticks and the pathogens that they carry are increasing in prevalence and distribution nationwide. According to the CDC 2018 study report, tick-borne disease cases more than doubled in the United States in 13 years and were 77 percent of all vector-borne disease reports.
Lyme disease accounted for 82 percent of those reports, and case numbers of other TBDs also increased. During this same time period, seven tick-borne diseases were reported for the first time in the United States. New species of ticks are being documented for the first time in the United States as well as in states not previously recorded.
Education and awareness of tick-borne diseases (TBD) is important for patients to both prevent disease and to be able to advocate for themselves if they are bitten or suspect a tick-borne disease. There is a nationwide need for clinicians to gain more in-depth education for rapidly growing health risks to consider tickborne diseases when evaluating patients. Outdoor workers, people that recreate in the outdoors, travel, or those who have close contact with domestic animals or wildlife are at higher risk. Children are also at higher risk, and symptoms of Lyme and other tick-borne diseases can appear differently, sometimes manifesting solely as neuropsychiatric symptoms.
Diagnosis of tick-borne diseases is often difficult. Nearly 50 percent of people that develop Lyme disease have no recollection of a tick bite. For children, this number is even less, below 20 percent. The ticks that most often transmit the germ that causes Lyme disease and many other TBDs can be the size of a pinhead.
Also challenging is the reliance on the presence of a rash to diagnose Lyme or other tick-borne diseases. Too often, clinicians and patients believe that the rash indicative of Lyme disease always presents in a bull’s-eye pattern. Many people that develop Lyme disease do not manifest or observe an expanding bull’s eye rash or erythema migrans (EM) rash, or any rash at all.
In a recent article of “The Spectrum of Erythema Migrans in Early Lyme Disease: Can We Improve Its Recognition?” it was found that out of 69 study participants with rashes that were suspected of early Lyme disease, only six percent were observed with a classic bull’s eye rash pattern. EM rashes, when present, commonly occur in forms that are not the classic bull’s eye. In this study, it was also found that most patients tested negative on currently available laboratory tests which adds to the challenge of confirming a Lyme disease diagnosis and complicates treatment decisions.
Reliance on the manifestation and recognition of a bull’s eye rash on darker skin tones can further delay diagnosis and treatment of Lyme disease for people with brown or black skin. This disparity creates inequity of disease recognition and care for those with brown or black skin. The CDC just released a new poster demonstrating the variability of Lyme rashes on various skin tones.
Other symptoms of tickborne diseases may appear as flu-like in the early stages of the disease including fever, severe headache and neck stiffness, fatigue, muscle/joint pain, nausea, diarrhea, vomiting, rashes of various presentations (spotted, streaked), swollen lymph nodes, and other symptoms that are similar to other illnesses, making diagnosis difficult especially when the history of a tick-bite is not noted. Laboratory tests for many tick-borne diseases are highly unreliable, especially in the early stages of disease, making diagnosis even more challenging.
Acute Lyme and other tickborne diseases may also present as serious and life-threatening illnesses including carditis, facial palsy, and encephalopathy. Some diseases can be fatal if not treated in the first few days. If tick-borne disease is suspected (Lyme carditis, Rocky Mountain spotted fever, etc), the earlier treatment is initiated, typically the better the outcome.
Many tick-borne diseases can also be transferred from an infected mother to her unborn child during pregnancy. The CDC states that it is “possible yet rare” for untreated Lyme disease to infect the placenta and spread from mother to fetus. The CDC stresses the importance of diagnosis and treatment during pregnancy. Research is lacking on the long-term outcome of children that may contract Lyme disease congenitally.
Colorado reported eight human cases of Lyme disease in 2019, the largest annually reported case number in the state’s history, and case investigations have been on hold due to limited capacity during the COVID-19 pandemic. Cases of Lyme and other tick-borne diseases in Colorado are likely underreported, due to limited education and prevention awareness, limited surveillance activities, and the difficulty of diagnosis.
When Lyme and other tick-borne diseases are not quickly and accurately diagnosed or treated, they may result in severe illness, chronic disabling symptoms, or death; and may mimic many other diseases, including acute and long-haul COVID-19. Various studies have found that 20 to 60 percent of patients that acquire Lyme disease may develop chronic or persistent symptoms.
Lorraine Johnson and Elizabeth Maloney, M.D. published “Access to Care in Lyme Disease: Clinician Barriers to Providing Care” in which they found that “Patients with persistent Lyme disease/chronic Lyme disease (PLD/CLD) encounter significant barriers to accessing medical care.”
Because of the complexities of symptoms and health issues for patients with chronic/persistent Lyme disease, many patients go years undiagnosed or misdiagnosed with progressively disabling symptoms and are often told that their physical symptoms are solely psychological in origin or “all in their head.” The controversy over the root cause of these symptoms has been plaguing patients and the clinicians that treat patients for over four decades and the science is still unsettled.
The best protection against Lyme and other tick-borne diseases/conditions is awareness, prevention, education, prompt and accurate diagnosis, and early and adequate treatment.
Colorado Tick-Borne Disease Awareness Association (COTBDAA), Chaffee County Public Health (CCPH), and Partnership for Community Action (PfCA) are partnering in this month-long awareness campaign.
- May 1: Kicking off the month is Moonlight Monday with donations going to support Colorado Tick-Borne Disease Awareness Association (COTBDAA) and the Chaffee County month-long awareness campaign. A prevention education table will be present at Moonlight Pizza and Brewpub for this event.
In partnership, COTBDAA, CCPH and PfCA are providing free community screenings of the breaking film, The Quiet Epidemic, a powerful documentary that is spurring a grassroots effort to expose the real impact of Lyme disease nationwide. - May 5: The Salida screening of The Quiet Epidemic will take place at the Steam Plant Theater. CCPH will be providing light appetizers and refreshments, and this screening will be followed by a panel discussion with the co-directors of this impactful film, Winslow Crane-Murdoch and Lindsay Keys, Lyme Literate medical clinicians, Dr. Julie Barter and Dr. Sharon P Austin, patients and advocates will also be part of this panel discussion with the community!
- May 10: The Buena Vista screening will take place at the Stardust Theater and will be followed by a Q&A with local health advocates and patients (snacks provided).
Both screenings are free and open to the public, and RSVP is kindly requested. Find details and RSVP at www.coloradoticks.org. - May 18: Salida Soup, hosted by PfCA, will be dedicated to COTBDAA and Lyme and Tickborne Disease/Conditions Awareness Month. A prevention education resource table will be present!
Additional Resources and Events:
- Link to CCPH website: https://www.chaffeecounty.org/Public-Health-Tick-Born-Disease-Prevention
- Link to COTBDAA: https://coloradoticks.org/
- Link to PfCA: www.gopfca.com
- Link to Looking Upstream: A We Are Chaffee podcast, with Adam Williams and Monica White https://www.wearechaffee.org/white
- Link to We are Chaffee Story of Resilience: “one little bite” https://www.wearechaffee.org/copy-of-community-stories
- Link to CCHC COTBDAA blog: https://chaffeeresources.com/staying-tick-safe-in-the-outdoors-by-monica-white/
- Link to The Quiet Epidemic Trailer: https://www.thequietepidemic.com/
- Link to Ticks and Tick-Borne Diseases of Colorado, Including New State Records for Argas radiatus (Ixodida: Argasidae) and Ixodes brunneus (Ixodida: Ixodidae): https://pubmed.ncbi.nlm.nih.gov/33164093/
Prevent Tick Bites:
Know your surroundings: Depending on where you live, work or travel ticks and tick-borne diseases may be different, more prevalent, and active at different times of the year.
Wear permethrin-treated clothing and gear
Tuck shirts into pants and long pants into socks, or wear gaiters
Use only EPA-approved tick repellants on exposed skin
Stick to the center of trails
Throw exposed clothing in a dryer at high heat for 10 minutes to kill any hitchhikers
Shower when you return indoors
Do tick checks: Use a mirror or a partner. Help check young children and check your pets too! Especially…
- Head & Hair
- Nape of neck and in and around ears
- Under arms
- Belly button and waistline
- Between legs and groin area
- Back of knees
- Between toes
If a tick is found remove properly:
- Use fine nosed (pointy tweezers)
- Grab tick as close to skin as possible and pull tick out with slow and steady motion
- Place tick in airtight container
- Disinfect the bite area, tweezers, and hands
- Consider sending the tick for identification and testing
- The time it takes for a tick to transmit germs that cause disease can vary from minutes to hours. The sooner the tick is removed, the better.






Thank you for posting this important information to help keep our community members well!