HRRMC in Solid Financial Health
The Heart of the Rockies Regional Medical Center (HRRMC) Board of Directors heard a review of the district’s financial condition from its accounting firm, FORVIS LLP, on Tuesday, March 28. The audit revealed that as Colorado rural hospital systems go, this rural medical provider is doing well.

Bob Morasko, CEO of Heart of the Rockies Regional Medical Center. Courtesy photo.
At the board meeting, CEO Bob Morasko said that HRRMC s doing much better than many other rural hospitals in the state.
“Rural hospitals are at risk now …,” said CEO Bob Morasko. “As I look around me and all the hospitals around us, it’s kind of unnerving for me, because I see what’s going on.”
Tammy Rivera of FORVIS made the detailed presentation, which generally found a “clean” audit, but made some suggestions for future accounting procedure improvements.
The bottom line summary said: “Clean unmodified opinion”.
In addition, FORVIS reported that the Audit Committee Letter was reviewed with the Finance Committee and there were “no material weaknesses or significant deficiencies.”
However, Rivera called attention to the implementation of the new accounting standard known as GASB 87. She said that some 2021 amounts have been restated for implementation of GASB 87, the significance of which has to do with subscription-based information technology and GASB 101, about accounting for compensated employee absences.
Commenting on fiscal crises at hospitals in Leadville and Delta, where even sales tax increases sometimes have not helped, Morasko said, “You look across rural Colorado and it’s a tough, tough environment. We’re so blessed to be where we’re at, financially, but it’s a lot of hard work with our staff …”
Tax revenue in the HRRMC service region provides about $750,000 annually for the district.
“We just have to stay progressive, keep our leadership team intact,” said Morasco. “We have a great leadership team, and that’s the difference, it really is – keep our employees stable, making sure our wages and benefits are competitive, which we have. We just have to stay progressive with recruitment and retention,” he added.
Key HRRMC Statistics
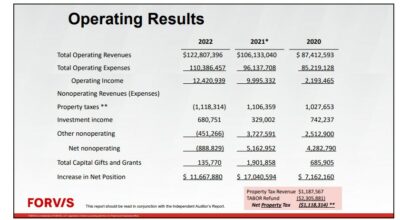
HRRMC Operating Results. Note $2.3 million TABOR refund payout to taxpayers. Image Courtesy FORVIS/HRRMC

HRRMC Margin of revenue over expense. Image courtesy FORVIS/HRRMC

HRRMC Deb Service Coverage Ratio shows growth over 2021. Image courtesy FORVIS/HRRMC
As the district navigates the third year of dealing with the COVID pandemic in 2022, it appears to have done well. Comparisons of the fiscal health of other hospitals in the state to HRRMC show that many facilities saw deep reductions in profit margins as costs escalated over personnel wages and benefits, supplies and equipment, charity care, bad debt, and investment declines from market downturns.
The Denver Post recently reported overall, most state hospitals were still profitable last year, citing a 4.7 percent profit margin for patient care. But that was before investment losses dropped that margin to about 1.5 percent. In 2019, that profit margin was tagged at 10.6 percent statewide.
The complex financial picture for hospitals in the state was exacerbated by lower rates paid by Medicaid and Medicare. With pandemic government aid and investments mixed in, hospitals still managed to hit respectable profit margins in both 2020 (8.6 percent) and 2021 (9.6 percent) according to the Post.
Still, some rural hospitals struggled. Six of eight hospital systems, the Post reported, had negative profit margins in the first nine months of last year, while five were profitable when only patient care was considered.
Most notably, St. Vincent Hospital in Leadville was nearly forced to close until state and local funds totaling $1.5 million were used to keep the doors open. The newspaper said Kaiser Health News pointed out that St. Vincent had expanded district services which proved to be unsustainable. It was also dealing with problem-plagued accounting software which adversely affected their billing system efficiency.
Another factor in status reviews for hospitals is investment income; basically how much ‘rainy day fund’ operating cash is on hand.
In addition, the Post reported that while state hospitals were profitable in 2020 and 201, part of the reason was funds approved as a stimulus to help the country handle the COVID pandemic. The paper pointed out that independent hospitals were less profitable than larger systems, and urban hospitals fared better than rural ones.
Rural independent facilities like HRRMC had a median of 215 days of cash on hand, while urban and system hospitals had about 245 days of cash on hand.
In 2022 HRRMC exceeded the average cash-on-hand performance of urban and system hospitals: it had 254 days of cash on hand, including investments, compared with 289 days of cash on hand in 2021.
The Post reported that the Colorado Hospital Association (CHA) indicated that for all state hospitals, patient revenue rose by about $898 million from 2121 to 2022. But at the same time, expenses for providing care soared by $1.7 billion (nearly half due to higher salary expenses, such as traveling nurses to fill positions impacted by ubiquitous employee shortages) as well as higher costs for supplies and other factors.





Recent Comments